Aortic Dissection (AD)
Aortic dissection is the most common catastrophe affecting the aorta. The aorta is the largest artery of the body through which blood leaves the heart to deliver oxygenated blood to the rest of the body.
What is Aortic Dissection (AD)?
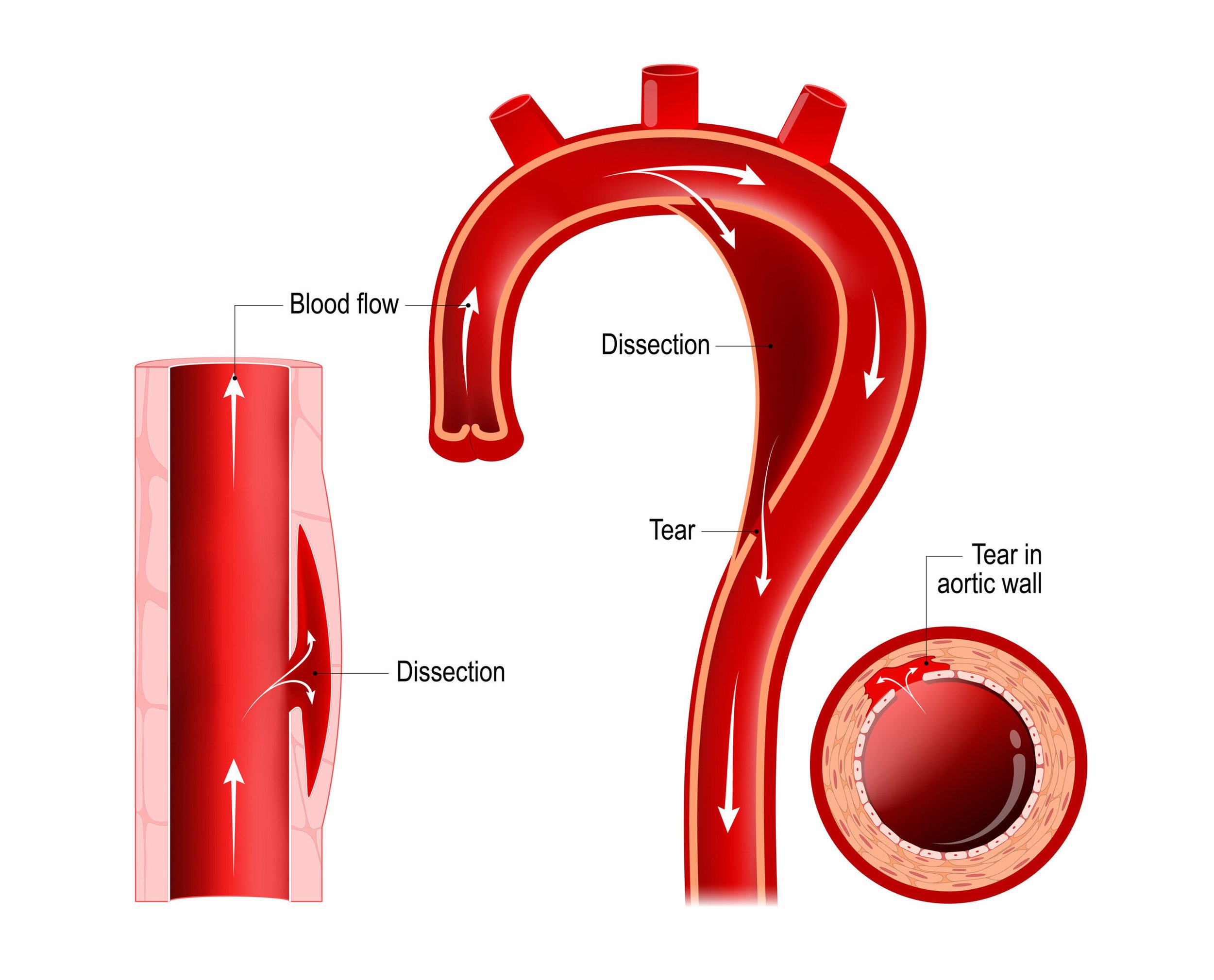
Aortic dissection is the most common catastrophe affecting the aorta. The aorta is the largest artery of the body through which blood leaves the heart to deliver oxygenated blood to the rest of the body. It occurs in about 24 people per million each year in the U.S. It is caused when the inner layer of the aortic wall tears and then peels or separates away from the next layer of the aorta. This creates two channels; the original aortic channel for blood flow (the true lumen) is still present while the peeling away of the outer layer in the dissection creates a new additional ow channel (the false lumen).
This double-barrel flow pattern in the dissected aorta can cause serious problems upstream or downstream from the tear. The dissection or separation can result in a significant decrease in blood flow to various organs and tissues supplied by the involved branches. Branches that may be affected include the kidney (renal) arteries, the gut (mesenteric) arteries, the arteries to the brain, and the arteries to the arms or legs. In addition, the tear may compromise blood flow to the heart causing a heart attack and in some cases can result in internal bleeding around the heart, causing loss of consciousness or death.
Aortic dissection is a very serious, life-threatening disorder that requires immediate medical attention.
Symptoms
Location of Pain:
Chest pain
Back pain
Flank pain
Abdominal pain
Leg pain
Quality of Pain:
Pain that is tearing or sharp
Abrupt onset of pain
Pain that migrates or radiates
Neurological Deficits:
Coma/Altered consciousness
Paralysis
Extremity numbness
Difficulty with speaking or slurred speech
Light-headedness/Fainting
Difficulty breathing/Shortness of breath
Diagnosis
When a physician suspects the diagnosis of aortic dissection, an imaging test is generally ordered to evaluate the aorta. There are three primary tests used to diagnose aortic dissection. Aortic dissection can be diagnosed with a CAT scan of the aorta or an MRI scan. A transesophageal echo (TEE) may also be performed. A TEE is a special type of ultrasound test during which a small ultrasound probe is passed through the mouth and into the stomach and esophagus to take very detailed pictures of the heart and aorta. Currently there are no blood tests that can accurately diagnose aortic dissection.
Early Diagnosis
When aortic aneurysms are diagnosed early, treatment is safe and effective and the aneurysm is curable. Aneurysms are often detected while performing tests for entirely different reasons. Most patients have no symptoms, so if you are at risk, it is important to discuss AAA with your doctor.
Causes
Proteins in the wall of the aorta, called elastin and collagen, provide strength and flexibility to this large artery. This is similar to muscles and tendons providing strength to the arms and legs. Aneurysms are caused by a progressive breakdown of these proteins that lead to a weakness of the wall of the aorta that can steadily expand like a balloon. These proteins, collagen and elastin, may gradually deteriorate with age.
Inflammation that is associated with atherosclerosis (hardening of the arteries) helps to accelerate this degenerative process even in younger people. Some of the body’s naturally occurring enzymes may also cause the breakdown of collagen and elastin in the wall of the aorta. An excess of these enzymes or conditions that activate the enzymes may cause the formation of an aneurysm, or lead to its sudden growth. In rare cases an aneurysm may be caused by infection. There is still much to be learned about the cause of aneurysms and their growth.
Treatment
In all cases, the first treatment for patients with aortic dissection is aggressive control of blood pressure with medications, usually given through an intravenous line (IV). Patients with aortic dissection are generally monitored in the intensive care unit. A team of experts cares for patients with aortic dissection, including emergency medicine physicians, cardiac and vascular surgeons, cardiologists, radiologists, and internal medicine specialists. The treatment of aortic dissection depends upon a number of factors, including the location of the tear in the aortic wall, how much of the aorta is involved, the effects of the dissection on the branch vessels of the aorta and the perfusion of the organs, and the patient’s symptoms. For patients with aortic dissection who require invasive treatment, surgery to repair the dissected portion of the aorta is generally the recommended treatment. In some cases, minimally invasive stenting procedures can be used to treat aortic dissection.
For all patients who have an aortic dissection long-term follow-up with a physician is a very important part of treatment. Blood pressure and heart rate need to be carefully monitored and controlled with medications. For many patients, CAT scans or MRI scans will be repeated at regular intervals (such as every 6 months or every year) to monitor the size of the aorta and the status of the dissection.
Risk Factors
The main preventable risk factor for an aortic dissection is high blood pressure (hypertension). Over time, hypertension weakens the aortic wall, making it more likely to have a spontaneous tear involving the inner lining of the aorta. The tear exposes the middle of the wall to very high aortic blood pressure. This creates a separation that unzips the aorta between the layers which are pulled apart by the dissection process, leading to the double-barrel flow pattern. Other risk factors for aortic dissection include: Marfan or Ehlers-Danlos syndrome, which are inherited disorders of blood vessels and connective tissues; presence of aortic aneurysm or enlargement of the aorta; a family history of aortic dissection; and certain heart conditions such as a bicuspid aortic valve. Aortic dissection may also occur as a complication of open heart surgery or heart catheterization, although this is very rare.
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.