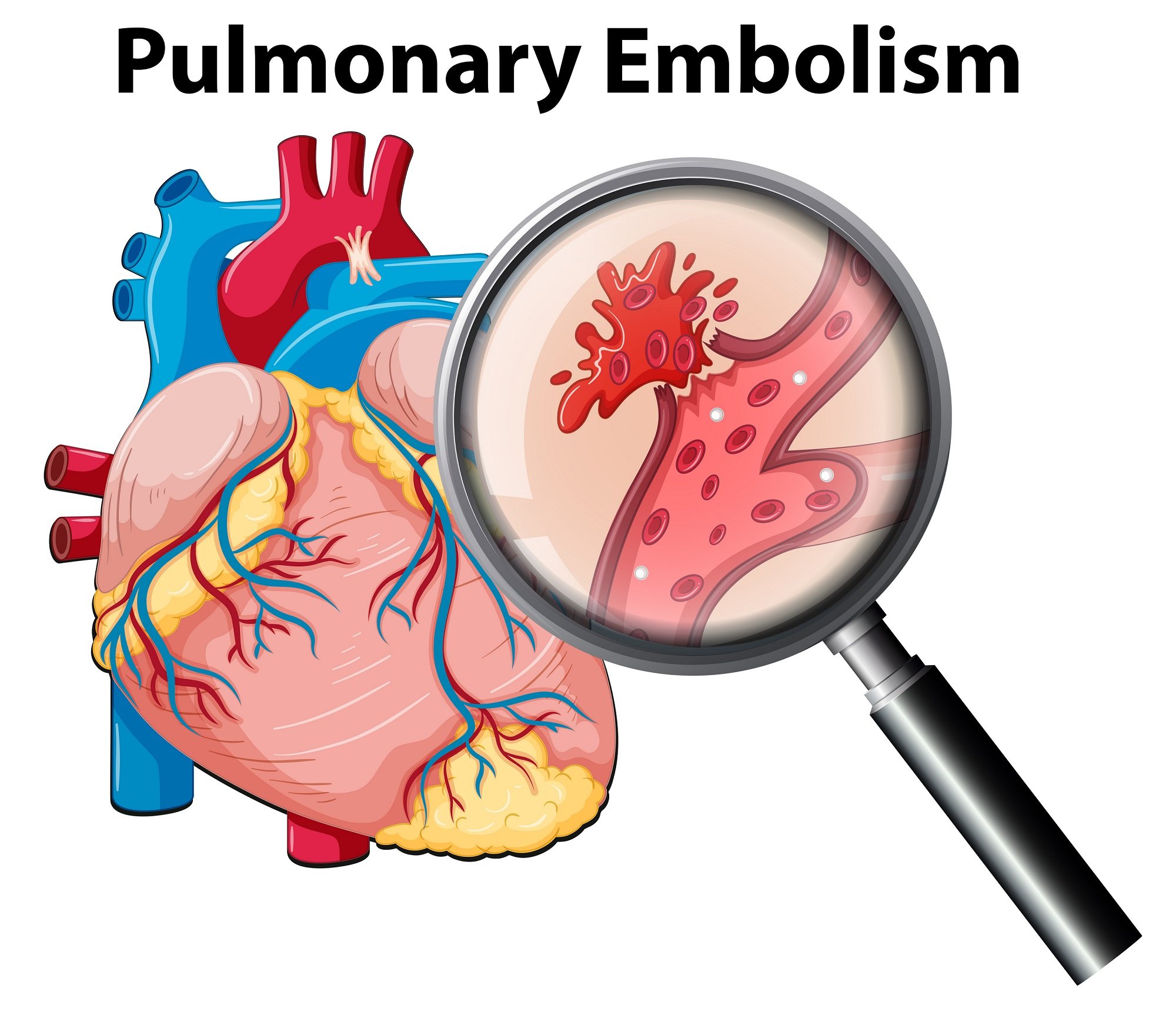
Pulmonary Embolism
A Pulmonary Embolism (PE) is a blood clot that lodges in the lung arteries. The blood clot forms in the leg, pelvic, or arm veins, then breaks off from the vein wall and travels through the heart into the lung arteries.
What is Pulmonary Embolism (PE)?
A pulmonary Embolism (PE) is a blood clot that lodges in the lung arteries. The blood clot forms in the leg, pelvic, or arm veins, then breaks off from the vein wall and travels through the heart into the lung arteries. Most PEs are due to pelvic and upper leg blood clots that first grow to a large size in the vein before detaching and traveling to the lungs. PE can cause death or chronic shortness of breath from high lung artery pressures (“pulmonary hypertension”). PE can impair heart muscle function, especially the right ventricle, which pumps blood into the lung arteries.
Most of the people who die from a pulmonary embolism do so within 30 to 60 minutes after symptoms begin.
Symptoms
The most common symptom is unexplained shortness of breath and/or chest pain with difficulty breathing. However, PE can be difficult to diagnose and has been called “The Great Masquerader.” It can mimic pneumonia, congestive heart failure, and a viral illness known as pleurisy.
Shortness of breath
Chest pain, often worse when taking a breath
A feeling of apprehension
Sudden collapse
Coughing
Sweating
Bloody phlegm (coughing up blood)
The signs and symptoms of these disorders can vary by individual and event. Some individuals may also experience uncommon symptoms such as dizziness, back pain or wheezing. Because PE can be fatal, if you experience these signs or symptoms seek medical attention right away.
Diagnosis
A definitive diagnosis of PE must be made in a hospital or clinic with radiology facilities. A chest CT scan (“CAT scan”) or a nuclear medicine scan are the most common tests to diagnosis PE. The most crucial point is for patients and their health care providers to consider the possibility of PE. Prior to a chest CT scan or a nuclear medicine scan, doctors may determine the likelihood of PE through screening tests such as a chest X-ray, electrocardiogram and a blood test called a “D-dimer” (low D-dimer levels virtually exclude PE).
Treatment
The foundation of treatment is thinning the blood with anticoagulants such as heparin, low molecular weight heparin, fondaparinux, direct thrombin inhibitors (argatroban, lepirudin, or bivalirudin) or the oral blood thinner, warfarin. Immediately acting intravenous or injected blood thinner must be administered right away. The oral blood thinner, warfarin, takes about five days to become effective to prevent the development of a recurrent PE.
In addition to blood thinners, more aggressive therapies include “clot buster” drugs such as TPA or catheter-based or surgical embolectomy to remove the PE.
The duration of treatment with the oral blood thinner will vary from 6 months to lifelong, depending upon the circumstances of the PE and other individual risk factors.
Prevention
Prevention of PE is a lot easier than diagnosis or treatment. Therefore, when hospitalized, it is important to ask your health care providers what measures are being taken to prevent PE. These can include the use of graduated compression stockings or prescription of low doses of blood thinners such as unfractionated heparin, low molecular weight heparin, or fondaparinux.
Surgeon General’s Call To Action
Members of the Venous Disease Coalition (VDC) and the Office of the Surgeon General came together at the VDC Annual Meeting in Washington D.C. on September 15th, 2008. Acting Surgeon General Rear Admiral Steven K. Galson issued “The Surgeon General’s Call to Action for the Prevention of Deep Vein Thrombosis and Pulmonary Embolism,” which combined affects hundreds of thousands of Americans each year. This announcement was made at the Venous Disease Coalition’s 2nd annual meeting. The VDC is an initiative of the VDF.
Dr. Galson laid out recommendations for the prevention of these two common, yet deadly major public health threats, deep vein thrombosis (DVT) and pulmonary embolism (PE). The Call to Action urges a coordinated, multifaceted plan to reduce the number of cases of deep vein thrombosis and pulmonary embolism nationwide. The plan emphasizes the need for:
Increased awareness about deep vein thrombosis and pulmonary embolism.
Evidence-based practices for deep vein thrombosis.
More research on the causes, prevention, and treatment of DVT.
“Together DVT and PE may be responsible for more than 100,000 deaths each year, but there is reason to believe that the true incidence rate could be significantly higher, as several studies suggest that these diseases are often undiagnosed.” said Dr. Galson. “One thing is undeniably clear – DVT and PE are major national public health problems that have dramatic, negative impact on the lives of hundreds of thousands Americans each year.”
Risk Factors
Risk factors include immobility, smoking cigarettes, being overweight, and having high blood pressure – all of which can be potentially controlled with a heart healthy lifestyle. A recent study showed that eating fruits and vegetables can be protective against developing PE. However, people who frequently eat red meat had double the risk of developing PE. Other risk factors for PE include cancer, long airline flights, surgery and trauma. PE is also associated with women’s health issues such as use of birth control pills, pregnancy and hormone replacement therapy. Certain genetic mutations predispose to PE, such as “factor V Leiden” and the “prothrombin gene mutation.”
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.