Diabetes and Vascular Disease
Diabetes is a disease in the body where blood sugar (glucose) in your body is too high. High blood sugar can increase your risk for vascular disease.
What is the link between diabetes and vascular disease?
Diabetes increases the risk for developing atherosclerosis. Atherosclerosis happens when arteries harden or narrow from a build-up of a fatty, stick substance called plaque. People who have diabetes may also have high cholesterol. The combination of both medical conditions can cause plaque to accumulate in the arteries at a faster rate.
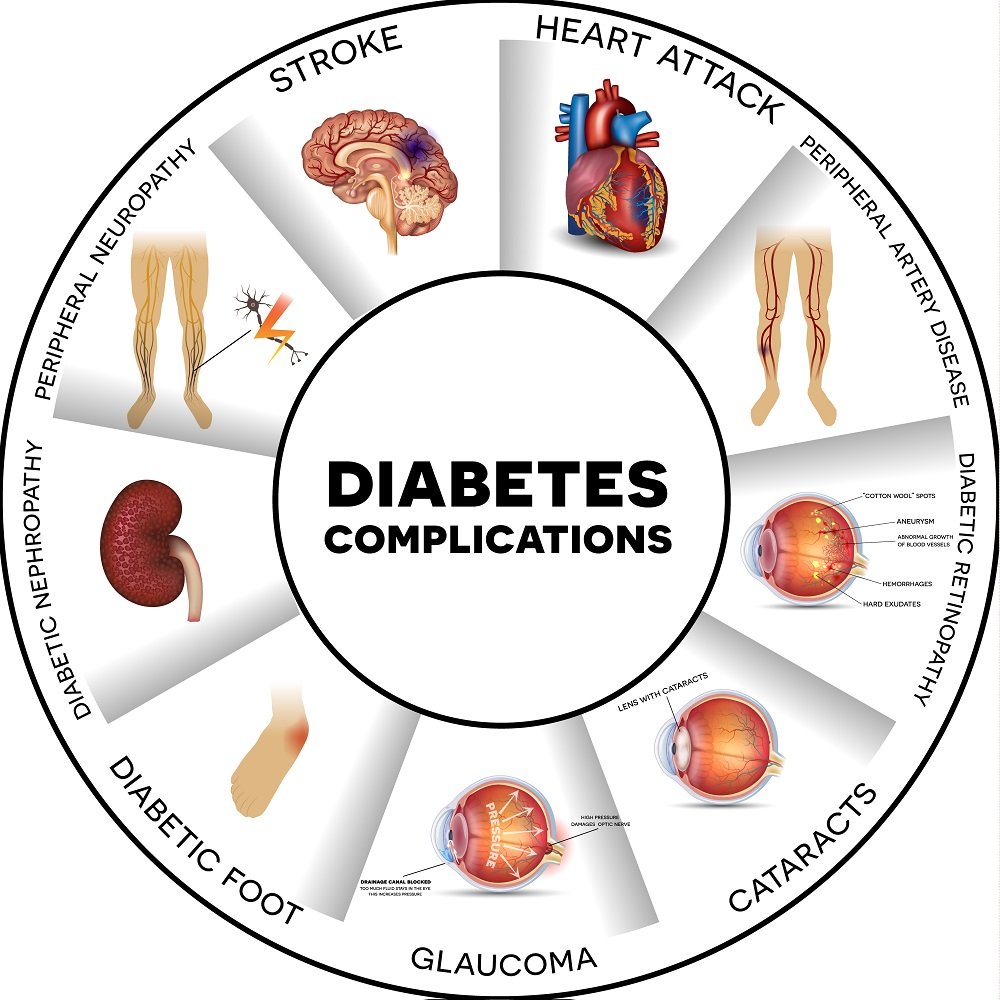
Diabetes can affect small and large blood vessels in different parts of the body:
Eyes: Diabetic retinopathy is a common eye disease that can lead to blindness. This condition is caused by damaged blood vessels in the retina (light-sensitive layer of cells in the back of the eye).
Kidneys: Over time, high blood sugar can damage arteries that supply blood to your kidneys. This is called diabetic nephropathy.
Heart: High blood sugar can eventually damage blood vessels around the heart. This can lead to coronary artery disease (CAD), which affects the blood flow to the heart. CAD leads to a higher risk of heart attack.
Peripheral Artery Disease (PAD): This condition mostly affects the legs and feet. As arteries in the legs get clogged, there is less blood flow from the heart. This can affect someone’s ability to walk and could lead to a greater risk for limb loss or amputation.
Diabetes and Peripheral Artery Disease (PAD)
People with diabetes are at a higher risk for Peripheral artery disease (PAD). But not a lot of people, including healthcare providers know about this disease. Studies have found that one out of three people older than age 50 who has diabetes also has PAD. PAD is also more common in Black and Latino populations.
Individuals who have both diabetes and PAD:
Have a lower life expectancy
Are at increased risk for a heart attack or stroke
Might not notice PAD symptoms right away, because people with diabetes have less feeling (or decreased sensation also known as neuropathy) in their feet
Experience slower wound healing due to decreased blood flow to the feet and legs
Are at higher risk for losing a foot or leg due to amputation
To find out more about the warning signs of PAD, visit our PAD Landing Page.
Ask your healthcare provider if getting tested for PAD is right for you. Testing for PAD is recommended for people with diabetes who are younger than 50. Even if you don’t have symptoms, it is very important to get tested if you have other risk factors, such as smoking, high blood pressure, or cholesterol problems.
Managing Diabetes & Lifestyle Changes
Diet
Many people think that having diabetes means you cannot eat your favorite foods. But you can still enjoy many of the foods you like. Portion sizes, or the amount of food you eat, affects your blood glucose. Ask your health care team to refer you to a dietitian who helps people with diabetes. The two of you will design a meal plan that is right for you and can help you reach your goals. Also keep the following tips in mind.
Count carbohydrates (also called carbs): Breads, tortillas, biscuits, rice, crackers, cereal, fruit, juice, milk, yogurt, potatoes, corn, peas, and sweet potatoes tend to raise your blood glucose levels more than other foods. Ask your health care team what amount of carbohydrates is right for you and how to keep your carb intake at a reasonable level.
Choose foods low in saturated fat: Cutting down on foods that have saturated fat can help lower your low-density lipoprotein (LDL, or “bad”) cholesterol and prevent heart disease. Saturated fat can cause blockages in your blood vessels. Foods low in saturated fat include fish that are high in omega-3 fatty acids (salmon, trout, sardines, and tuna), lean beef, lean pork, chicken breasts, ground turkey, and avocados.
Losing Excess Weight
Managing or losing extra weight can be challenging, but it is possible with support and a plan that works for you. It is important to be kind to yourself and take it one step at a time. Here are a few tips that may help get you started. Remember: Before starting any weight-loss plan or diet, check in with your healthcare provider to make sure it is safe for you.
Get at least 30 minutes of aerobic exercise each day. Examples of aerobic exercise include walking briskly, dancing, rowing, swimming or water aerobics, and biking. It is OK if it takes several weeks to build up to a practice of 30 minutes daily. The most important thing is to be physically active. Daily physical activity helps lower your blood glucose and blood pressure and control your cholesterol levels. Your health care team may want to check your heart function before you start new activities. They can help you plan the exercise program that is best for you, especially if you have pain in your legs when walking or during other physical activity. • Track your meals. Research shows that being mindful of what you eat can help you trim calories. Try writing down what you eat each day.
Make more meals at home. Cooking meals at home is an easy way to cut back on excess calories. Dining out or ordering fast food makes it harder to control the amount of cholesterol, salt, and fat in your food.
Increase the fiber in your diet. Your diet should include high-fiber foods, such as fruits, vegetables, dried beans and peas, oatmeal, and whole-grain breads, cereals, and pasta.
Medicines
Some people need medication as well as meal planning and physical activity to reach their blood glucose, blood pressure, and cholesterol targets—at least at first. Talk with your health care team about whether you need medications, and if so, which ones would best help you reach your goals.
Other Ways to Monitor Yourself and Stay on Top of Your Health
Check your feet every day for cuts, blisters, red spots, and swelling. Call your health care team right away about any sores that will not heal. Also, ask your health care team to check your feet at every visit.
Get an eye exam each year to check the blood vessels in your eyes for any early warning signs of damage. Contact your health care provider if your eyeglass prescription changes within a year.
Have your urine tested each year to check how well your kidneys function.
Get a flu shot every year and a pneumonia vaccine at least once to prevent being hospitalized if you get sick. When you turn 65, you should get another pneumonia vaccine, unless you have had one in the past five years
Risk Factors
Family history
Race or ethnic background
Age
Diabetes during pregnancy
Carrying excess weight
Sedentary lifestyle
High blood pressure
High “bad” cholesterol levels
Smoking
Heavy alcohol use
High stress levels
Not getting enough sleep
Resources:
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.