Peripheral Artery Disease
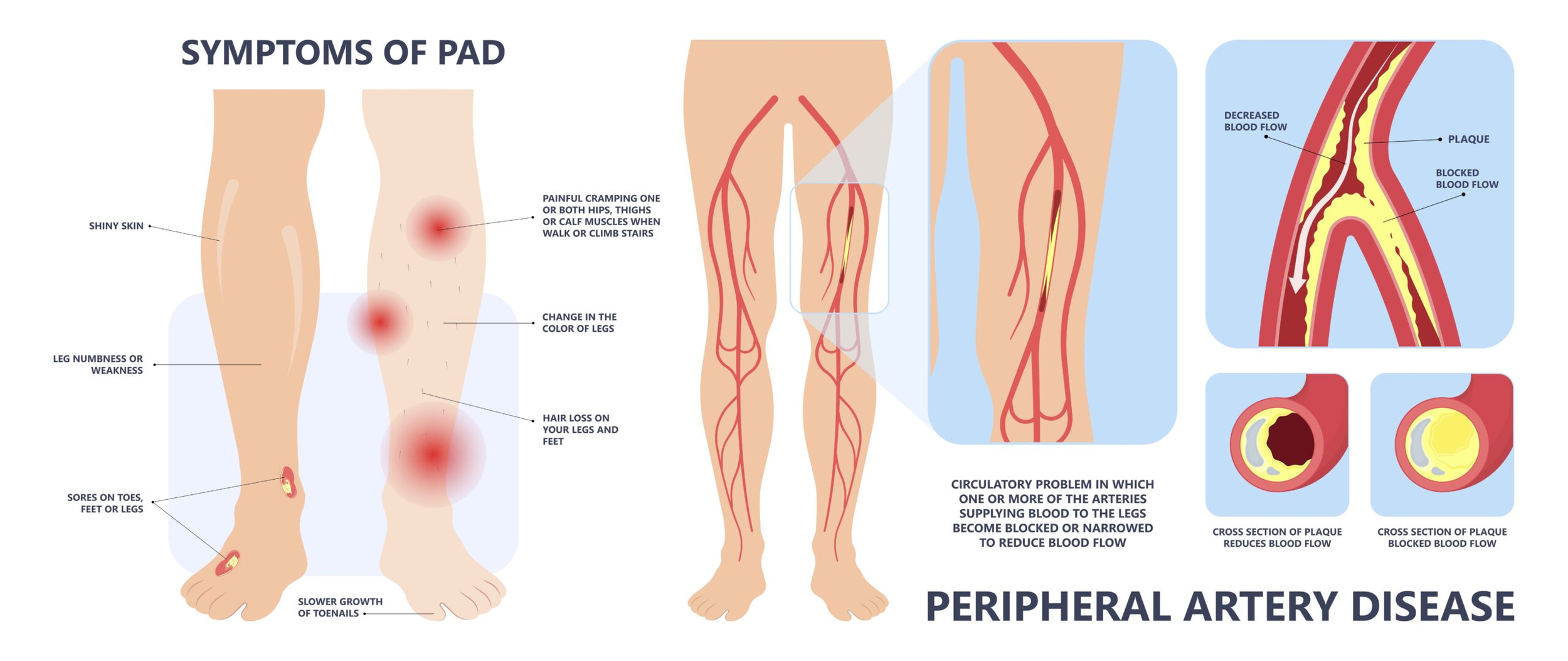
Peripheral Artery Disease results from a progressive thickening of an artery’s lining caused by a buildup of plaque, which narrows or blocks blood flow, reducing the circulation of the blood to a specific organ or region of the body.
Peripheral Artery Disease is a condition that affects millions of people.
Peripheral Artery Disease or PAD occurs when there is a buildup of plaque, or fatty deposits, inside the arteries that carry blood to your legs and feet. Many people have not heard of this condition. PAD often goes unnoticed because people assume their leg pain is due to soreness or arthritis. However, if your legs are healthy, you shouldn’t have chronic leg pain. Be aware that this condition doesn’t always present with symptoms, so it’s important to understand the risks and why you should get screened and diagnosed as soon as possible. If left untreated, PAD can cause amputations of the toes, feet, and even legs. Watch this video to learn more.
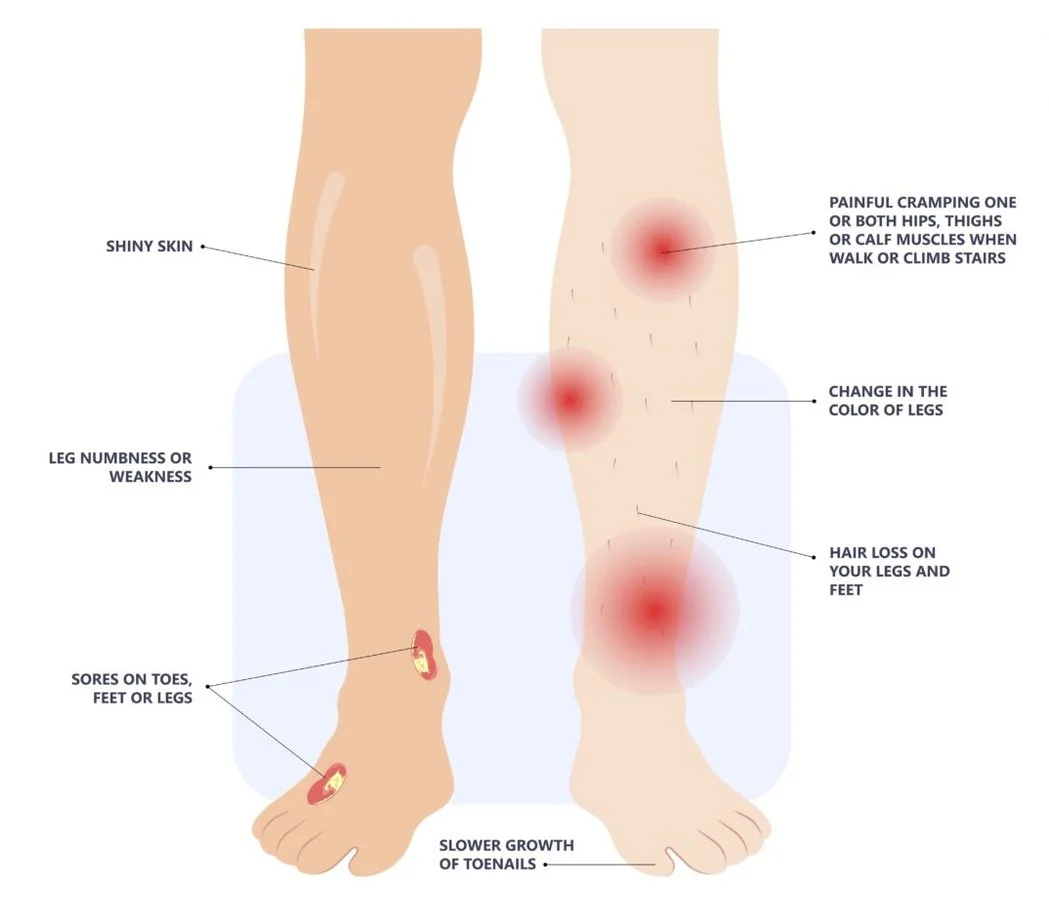
Symptoms of PAD
Here are some factors that increase your risk for PAD:
Increasing age (e.g. over 60)
High blood pressure
Diabetes (both Type 1 and Type 2)
Smoking
High blood cholesterol
It’s important to note that while these factors might increase your risk, PAD can develop even if you exercise and eat well. Certain communities, such as African-Americans, are at an increased risk for PAD.
What are the symptoms of PAD?
The most common symptom is cramping in your leg muscles while you’re walking. Pain that goes away when you stop and rest is called intermittent claudication. This is caused by poor blood flow to muscles due to blocked arteries.
Other symptoms of PAD include:
Burning or aching pain in your feet and toes while resting or sleeping
Skin sores and wounds that won’t heal
Nails that don’t grow
Hair loss on legs
Pale or discolored leg or foot
Changing skin color on your legs
Both legs often have symptoms, although one leg may be worse
Patient Stories
-
Hear from our Patient Partner, Steve
Walking changed his life and helped him treat his PAD.
-

Mechket learned to take control of her health
Mechket was diagnosed with an advanced form of Peripheral Artery Disease. Her diagnosis changed her life.
-

Bill’s Experience Getting a Second Opinion
Patient Partner Bill explains how he asked for a second opinion after surgery was recommended for his PAD.
“When I came across Vascular Cures I learned a lot – I had never heard of PAD before. I only related losing limbs to diabetes. They actually saved my life.”
“Don’t be afraid to share your story. I felt, as a wellness coach, that I was supposed to be in perfect health and not have anything wrong with me. I have a platform to share my story on now, and I think we need to do a whole lot more. We need to get the word out about PAD in any way we can.”
“The most frustrating thing about having PAD is feeling helpless because you do not know what to say. If I were advising patient to patient, I would say; no one knows your body as you do. When it comes to your health, everything is essential.”
How is PAD Treated?
-
Going for walks, even short distances will help. Check out our walking resources page for tips on getting started. Ask your healthcare provider about an exercise program that’s right for you.
-
Smoking causes blood vessels to narrow and makes PAD worse. Reducing or quitting smoking can make a big difference in the treatment of PAD. See our downloadable flyer on PAD and smoking here.
-
Medications, such as statins (lowers cholesterol), antiplatelets (helps prevent clotting), and ACE inhibitors (lowers blood pressure), can be used to treat PAD. Speak with your health care provider about the best treatment option.
-
Your health care provider can refer you to a nutrition specialist or dietitian. They will help you find an eating plan that will not only help prevent PAD from getting worse, but can also reduce risk for heart attack and stroke.
-
Work-related stress, job strain, or other types of stress can make PAD worse. Stress may increase inflammation and cause higher blood glucose levels. Staying active, practicing meditation, or keeping a journal to track your moods can help relieve stressful feelings.
-
Some patients have severe cases of PAD that impact their quality of life. They are unable to walk long distances or have difficulties performing daily tasks. There are many surgical procedures that can help. For example, angioplasty helps open blocked arteries, and an artery bypass can help redirect blood around a section of partially blocked or fully blocked arteries.
Talk to your provider as soon as possible about your risk for PAD.
The sooner this condition is found, the more opportunity you have to control it.
Identify your PAD symptoms before your next provider visit.
We understand that sometimes it can be challenging to communicate your symptoms during your doctor’s appointment. Stand Against Amputation offers a PAD assessment quiz that you can print and bring to your next MD visit. Find out more here: Symptom Quiz.
Need help understanding your treatment decisions?
Show Me PAD is a decision aid for patients with peripheral artery disease. This resource helps patients become better informed to help them work with their provider in choosing PAD treatments that are right for them.
Want advice on advocating for yourself at the provider's office?
The Close the Gap initiative has resources in English and Spanish that help certain underserved communities, like women, Black adults, and Hispanic adults better understand how to communicate their needs at the provider's office. Check out the PAD resources here.
Resources
Educational Flyers
Learn More about Peripheral Artery Disease
Health-related information on this website including text, graphics, images, and other material is for educational purposes only and therefore not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately.