Chronic Limb-Threatening Ischemia
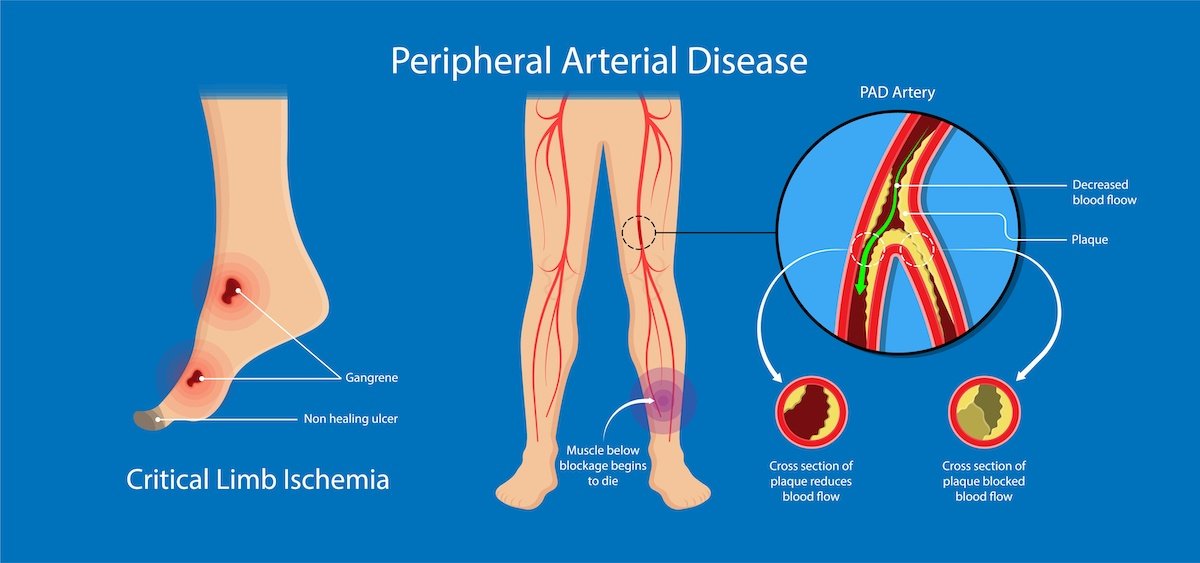
Chronic Limb-Threatening Ischemia (CLTI) was previously called Critical Limb Ischemia (CLI). CLTI is the end-stage of Peripheral Artery Disease (PAD). It is a severe condition that increases the risk for limb loss or major amputation.
Critical Limb Ischemia is Now Chronic Limb-Threatening Ischemia
Critical Limb Ischemia was renamed Chronic Limb-Threatening Ischemia (CLTI) in 2019. The name CLTI better reflects the broad range of patients with reduced blood flow that can delay wound healing and increase amputation risk.
What is Ischemia?
Understanding CLTI begins with ischemia (i-ski-me-ah). Ischemia is a severe condition in which there is not enough blood flow and oxygen to a part of the body. Without blood, cells and tissues begin to die, causing damage to parts of the body. Ischemia can occur anywhere blood flows. This includes the limbs, heart, brain, or intestines. A narrowing or blockage of an artery usually causes it. Signs and symptoms of ischemia depend on how quickly the blood flow is interrupted and where it occurs. This condition won’t improve on its own and requires medical attention by a vascular surgeon or vascular specialist.
Ischemia in the Legs
Ischemia can cause claudication anywhere from the hips to the toes in people who have peripheral artery disease (PAD). Claudication is pain in the calf, thighs or buttock that occurs with physical activity because of a lack of blood flow. It gets better with rest.
Claudication can progress over time to chronic limb-threatening ischemia (CLTI). This is severe pain or tissue loss due to the reduced blood flow to the affected limb. A non-healing sore or even gangrene (tissue death) may occur, causing the skin to turn black. A rapid decrease in blood flow to the legs may cause:
Severe pain
Loss of pulses
Coldness of the limb
Paleness of the skin
Leg weakness
Loss of sensation
Warning Signs of CLTI
Severe pain or numbness in the legs and feet when not moving
A noticeable decrease in the temperature of the lower leg or foot compared to the rest of the body
Toe or foot sores, infections or ulcers that will not heal, or heal very slowly
Gangrene, or dead, black tissue.
Shiny, smooth, dry skin in the legs or feet
Thickening of the toenails
Absent or weak pulses in the legs or feet
If you think you may have chronic limb-threatening ischemia or gangrene, and are experiencing any of the symptoms above, seek medical attention immediately.
Diagnosis
Diagnosis of ischemia depends on where it is in the body. The first clue is your symptoms. Monitor and write down your symptoms to discuss them with your healthcare provider. Your provider will ask you:
When and where the pain occurs
How often you get it
What relieves it
What makes it worse
If you feel discomfort and pain in your legs while walking, you may need to go to a noninvasive vascular laboratory. Here, you may have an ankle-brachial index (ABI) test. This tests the blood pressures in the legs. Depending on those findings, you may be sent for other diagnostic tests, such as:
Duplex ultrasound imaging of the arteries
A magnetic resonance arteriography (MRA)
Computed tomography (CT)
To see whether you have CLTI, your provider may order an arteriogram. This procedure takes images of your arteries. A special dye is injected to help the specialist see inside the arteries.
Treatment
CLTI treatment depends on a person’s medical history and their symptoms. Treatment is focused on getting more blood supply to the affected area as soon as possible. An earlier diagnosis leads to earlier treatment and better health outcomes. It is critical that someone with ulcers, or pain in the legs or feet when walking or at rest to see a vascular specialist right away. Quitting smoking is essential to improving blood flow and reducing the risk of amputation. If you smoke, it’s crucial to discuss a smoking cessation program with a healthcare provider. Other ways that CLTI is managed or treated include:
Medications:
Medicine is prescribed to prevent CLTI from getting worse. The goal is to reduce clotting risk and improve blood sugar, blood pressure and cholesterol. Medicines that fight infections and pain medications may also be prescribed in some instances.
Recommended surgical treatments for CLTI:
CLTI can be treated with revascularization (creating new ways around or through blocked or narrowed arteries). There are two common types:
An endovascular (meaning inside the blood vessel) procedure that involves an insertion of a thin flexible tube (catheter) through a narrowed artery. This catheter has a small balloon at the end and is inflated against the artery wall to improve blood flow.
A bypass surgery which involves a vascular surgeon using leg vein and connecting it to healthier arteries above the blocked arteries (vein graft).
Risk Factors
Smoking
Advanced age
High cholesterol
High blood pressure
Peripheral Artery Disease
Diabetes
Family history of cardiovascular disease
Sedentary or inactive lifestyle
Carrying excess weight
Resources
Be The Voice For Patients Like You!
Vascular Cures is inviting patients and advocates to share their stories, advise on our programs, and help us advocate for patient needs. Patients as Partners is a community where patients are heard, empowered, and encouraged to impact the health system. Learn more and request more information here.